How to Heal from PTSD

Post-Traumatic Stress Disorder (PTSD) first drew widespread attention when so many American combat veterans of the Vietnam War came back haunted, fearful and anxiety-ridden, unable to stop reliving the horrors of the war. Some retreated from society, others abused drugs or alcohol or became violent. Many committed suicide. Other symptoms include depression and insomnia. Most people have the ability to cope with everyday stress in a way that makes them still feel like they’re in control. Trauma, however, changes the way you see the world and destroys your sense of safety.
PTSD is described by great emotional upheaval and the shattering of the soul.
Glenn R. Schiraldi
Trauma Can Come Fast or Slow
According to Glenn R. Schiraldi in The Post-Traumatic Stress Disorder Sourcebook, PTSD is considered an anxiety disorder. It affects people who experience severe trauma, not just in war. This can include natural disasters, car crashes or assault. First, someone experiences an overwhelming, shocking event. Because it so shocks the conscience, they don’t fully feel the horror of it. The experience triggers a fight, flight or freeze response, flooding the body with the stress hormone cortisol, which impairs rational thought. They feel anxious and uncertain. They lose self-confidence and no longer feel safe, even after the event is over. They brush aside these feelings of powerlessness in order to meet their responsibilities while suppressing remembrance of the experience. Traumas inflicted intentionally by other humans, such as rape, cause the most severe PTSD reactions. Most often a traumatic event is a sudden, isolated experience, but it can also be chronic over a long period of time. About 70% of Americans will live through at least one such event in their lives.
Trauma short-circuits the brain’s ability to cope. Instead of processing the experience emotionally, people with PTSD avoid facing the memory at all costs, which then causes them to endlessly relive it. Seemingly random cues can trigger panic or a vivid flashback, and throw the sufferer’s nervous system into high alert so they remain hypervigilant. Or they can appear emotionless and pessimistic. PTSD sufferers experience a dissociative state where their brain effectively shuts down to avoid painful thoughts and feelings and then isolates traumatic memories. Instead of becoming mentally integrated as part of a person’s past, the memory remains ever-ready to intrude in the present. If a traumatic event made someone feel helpless, when PTSD kicks in, so will that feeling of helplessness. Dissociation takes a toll on your energy, leading to fatigue and preventing healing.
PTSD is a normal response to an abnormal event.
Glenn R. Schiraldi
As Jamie Ducharme points out in his article “Watching War Unfold on Social Media Affects Your Mental Health,” social media makes it easier for people to experience traumatizing events in vivid and visceral ways – even if they aren’t present – and it can affect their mental health.
Watching War Unfold on Social Media Affects Your Mental Health
time.comStudies show watching endless crisis news has a more harmful impact on mental health than the original crisis. Those watching six or more hours of news related to the 2013 Boston Marathon bombing reported higher levels of stress than people who were on-site during the explosions. Reading the news rather than watching graphic, unfiltered (and possibly fake) images on social media mitigates its toxic effects.
Sometimes trauma is more subtle, and also more chronic, embedded in circumstances like racism or sexual harassment. The effects of this persistent type of trauma are harder to recognize. In Trauma to Triumph, authors Mark Goulston and Diana Hendel caution businesses not to underestimate the trauma the COVID-19 pandemic caused their workers. The first step is to acknowledge the impact. When trauma goes unnamed, it can’t heal.
Naming, claiming and framing trauma helps us understand what is happening to individuals and to the group.
Mark Goulston and Diana Hendel
In Why Cope When You Can Heal, Goulston and Hendel focus on healing the trauma that health care workers on the front lines fighting the pandemic experience. The onslaught is daily, life-threatening and without an end in sight. Workers lack the support they need to do their best and are unable to take a break from the ceaseless experience of death they cannot forestall. This leads many to PTSD and persistent feelings of despair and helplessness. Many feel a “moral injury” similar to the experience of combat veterans. Add to that the adversarial mind-set many people now have toward healthcare workers and guidelines, and the experience is continually fraught and overwhelming. Despite the heavy psychological burdens of their job, frontline health care workers are not able to take the time to properly process their emotions. These workers experience high burnout and suicide rates.
For many, the PTSD they suffer is not noticeable. It could be the result of deeply buried childhood trauma. They seem fine interacting with others yet are emotionally detached or hypervigilant. They may experience flashbacks or intrusive thoughts. The trauma they’ve experienced makes them feel afraid and despairing.
Experiencing trauma often shatters your previous sense of safety and security. It can change the way you look at the world. And it can create lasting harms.
Mark Goulston and Diana Hendel
The Delayed Effects of Childhood Trauma
According to Robert Maunder MD and Jonathan Hunter MD in Damaged, 60 million adult Americans suffer the debilitating effects of childhood trauma. The reality of familial abuse is far more nuanced than “victims and villains.” The Adverse Childhood Experiences study showed people with higher scores were at greater risk for teen pregnancy, compulsive eating and obesity, risky behavior and substance abuse. They’re more vulnerable to heart, liver and lung disease. They die younger. Despite these health effects, doctors rarely ask their patients about childhood trauma.
With therapy, adults can recognize the harmful effects of their childhood traumas and cycles of abuse can end. But positive results depend on access to care and good quality relationships to bring about healing. Medical professionals can help their trauma patients by acknowledging their difficult past and how they adjusted to survive its harms. Emphasize continuity of care to resolve deep-seated trauma.
People whose early experiences have caused lifelong damage need a revolution of relationships, specifically a revolution of health care relationships.
Robert Maunder MD and Jonathan Hunter MD
In Lost Connections, Johann Hari recounts how Kaiser hospital doctors adopted the policy of asking patients about childhood trauma on their questionnaire, then giving them the option to discuss it with them. Just this simple acknowledgment and validation reduced doctor visits by 35%. Acknowledging the emotional connection to physical ills helps many people process their trauma. Hari also writes about the success patients have with alleviating depression by finding ways to reconnect with nature.
Evidence suggests that by reconnecting a person with his childhood trauma and showing him that an outside observer doesn’t see it as shameful, you go a significant way toward helping to set him free from some of its negative effects.
Johann Hari
Building a More Resilient Brain
Some people are better at handling adversity; they’re more resilient. Laura Moreno-Lopez, PhD, studies the brain scans of adults with childhood trauma in their past. Some of her subjects developed mental health problems while others healed and were able to live a normal life.
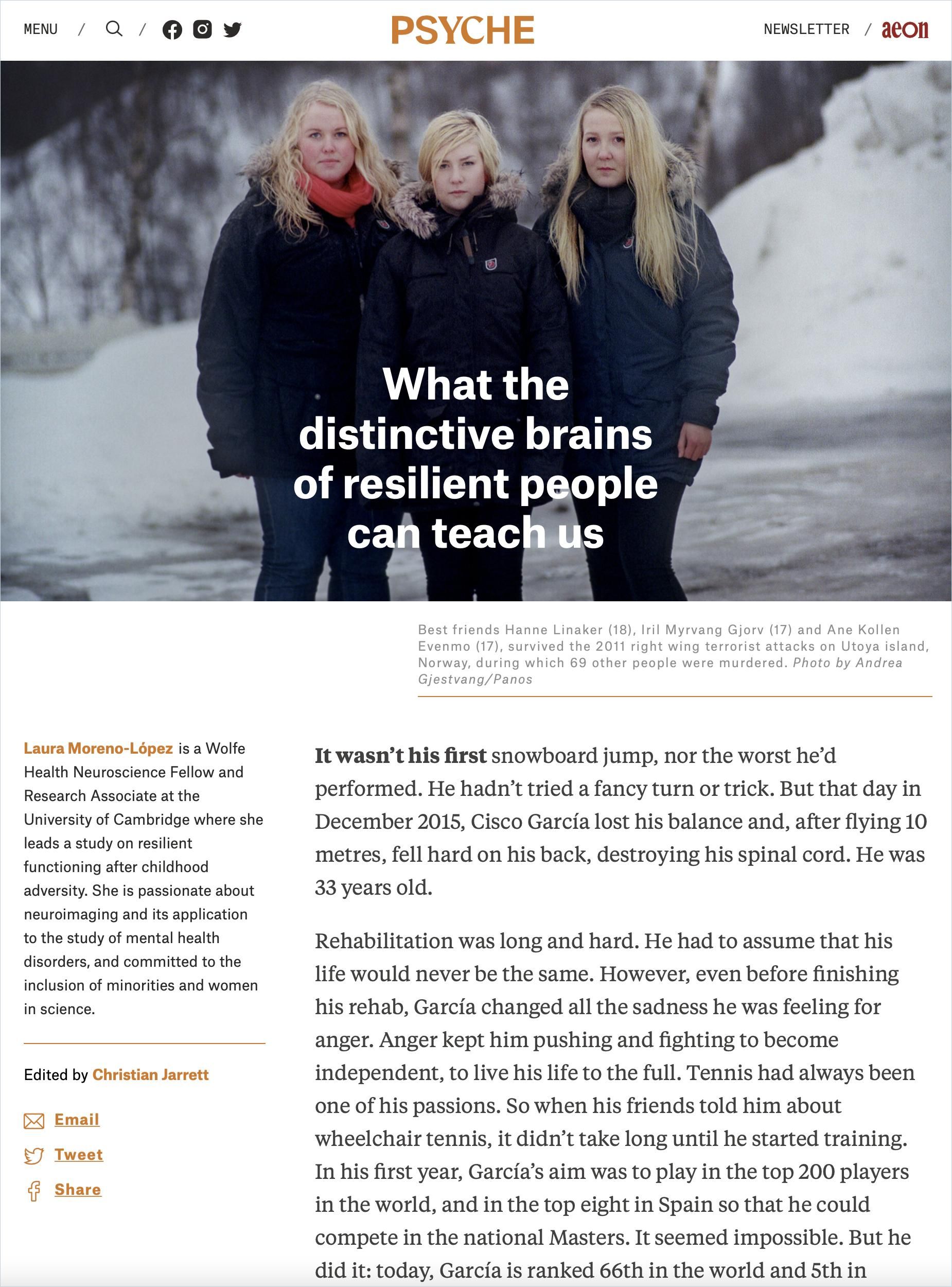
The science indicates a neurobiological basis for overcoming traumatic events in a healthy way that keeps PTSD from setting in. Brain scans show the most naturally resilient people have distinctive neurological characteristics, for instance, more solid connections between the “salience network” and the prefrontal cortex, which helps in the integration of facts and emotions. These differences point to strategies and therapies that anyone can use to build resilience. Although humans default to negative thoughts, more resilient people focus on the positive. People with childhood trauma can avoid depression by learning to call up positive thoughts and memories.
How to Heal
To finally heal their psyche, people with PTSD need to re-experience the trauma and process the negative feelings they’ve buried with the help of a professional. Talk with a therapist or join a support group. The empathy of others is healing. Focus on health by improving nutrition, exercise and relaxation. Effective treatments include:
- Cognitive Behavioral Therapy (CBT) entails working with a therapist to replace negative thought patterns with more positive ones.
- Eye Movement Desensitization and Reprocessing (EMDR) combines CBT with eye exercises that facilitate processing traumatic memories.
- Dialectical Behavior Therapy (DBT) focuses on fostering mindfulness and increasing distress tolerance.
- Somatic Experiencing Therapy is body-based and focuses on resetting the dysregulation of a patient’s autonomic nervous system.
- Tapping Therapy is an eastern approach where you tap different places on your body while recalling a traumatic memory; it’s a way to remain in connection with your body.
- Medication can help arrest debilitating symptoms like depression.
Review Your Organizations Crisis Management Plans
Organizations can experience traumatic events. Leaders rarely understand or deal with the impact trauma has on their employees or on the entire organization. Traumatic events can be violence, a sudden death or accident, natural disaster or sweeping layoffs. Goulston and Hendel list these as signs of organizational trauma:
- “Communication breakdown” – As leaders balance transparency and privacy issues, rumors circulate concerning the event.
- People look for where to assign blame. Was the accident preventable?
- People feel guilty for missing signs or surviving the trauma.
- People choose sides; this is common in cases of sexual harassment.
- Nobody talks about the trauma, which creates cultural dysfunction.
Organizations in crisis need strategies in place to get assistance to those directly affected and address the experience organizationally. It’s comforting to workers to know there are plans in place in case of disaster. Such plans should head off misinformation and emphasize organizational unity. Prepare plans for both sudden events and more slow-rolling events, such as a pandemic or mass layoffs. Leaders must offer hope while not downplaying people’s experiences. Bearing witness is a powerful way to stay present for others. Provide transparency, clarity and minimize uncertainty.
Logically, if you can’t survive today, you won’t be around tomorrow. But when the decision does not take the long view into consideration, that future is damaged.
Mark Goulston and Diana Hendel
When COVID-19 first hit, many leaders rose to the occasion to respond appropriately and protect workers. It made many companies review their crisis management procedures. At first, everybody pulled together to stop the spread of the virus, but as financial hardships multiplied and the pandemic wore on, sharp divisions arose. One side wanted to continue the lockdown and the other side wanted to end it in order for the economy to rebound. Parties politicized these views. Without a national plan, states came up with their own, causing spikes in the virus and decidedly not improving the economy. Had a plan been in place, leaders would have known how to guide the country forward, keeping people safe without tanking the economy. The dichotomy was false to begin with. Balancing competing objectives is routine for organizations, but trauma causes more dramatic fissures and hamstrings effective action. Managing emerging polarities well protects culture and productivity. To maintain stability, hold a debriefing session and encourage employees to talk about what happened, discuss the organization’s response, and speak honestly about how it could be improved. Be willing to facilitate difficult conversations.
Read more about preparing rapid response plans to crisis: