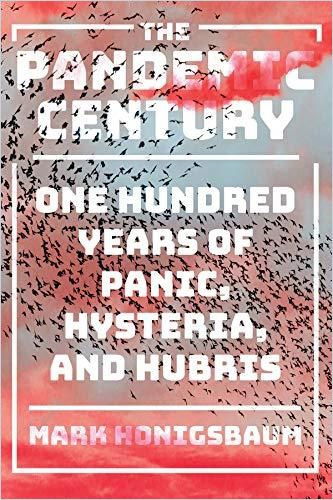
Prolific medical historian Mark Honigsbaum provides a chilling, detailed overview of the human experience of pandemics, encompassing plague, flu, SARS and AIDS.
Epidemics, Outbreaks and Pandemics
Medical historian Mark Honigsbaum, a lecturer at University College London, spent a decade researching modern plagues and pandemics, from the 1918 flu to AIDS and SARS. He believes more pandemics are coming. Honigsbaum’s thorough report predates the COVID-19 pandemic, though he pretty much predicts it.
Describing previous epidemics and pandemics, where and why they originated, how they spread, how and why governments and public health authorities responded to them, and what eventually contained them, Honigsbaum offers a road map to understanding and coping with COVID-19. He believes that the factor that makes a pandemic most dangerous is human ignorance; his historical account provides a powerful tool for those willing to be educated.
SARS
In early 2003, Honigsbaum reports, a Chinese bat likely infected a civet in one of China’s “wet markets,” where live animals sit side-by-side in cages waiting for someone to buy, butcher and eat them. The bat may have carried the virus – severe acute respiratory syndrome coronavirus (SARS-CoV) – that caused severe acute respiratory syndrome (SARS).
One of the major dangers arising from the effective control of SARS is complacency.Mark Honigsbaum
The virus infected a Chinese businessman who checked into Hong Kong’s Metropole Hotel in February 2003 and contaminated surfaces and the air for hours. SARS eventually infected 8,422 people in 30 countries, killing almost 1,000. Scientists isolated the virus, and then developed and distributed test kits. Containing SARS provided a false and dangerous sense of security regarding future pandemics.
“Spanish Flu”
During World War I, the United States built enormous camps to house tens of thousands of soldiers from farms and cities, including both recent immigrants and American-born. Their intermingling led to epidemics of bacterial diseases, including measles and pneumonia, and gave rise to the first wave of the worst pandemic in human history – the 1918 Spanish flu. More than 650,000 Americans – troops and civilians – succumbed, along with 100 million people worldwide.
A successful virus, Honigsbaum emphasizes, does not want to kill its host. It wants to spread.
Parrot Fever
Parrot fever spread across the United States (which had a major outbreak in 1929), Europe and Africa. The highly contagious disease transmits through the air in dried bird droppings. Scientists discovered that the main culprit was California-bred parakeets and songbirds.
Most cases of disease emergence can be traced to the disturbance of ecological equilibriums or alterations to the environments in which pathogens habitually reside.Mark Honigsbaum
Scientists again observed that bacterial and viral parasites in animals stay in equilibrium for centuries, but when people upset the ecology, then epidemics or pandemics emerge.
Legionnaires’ Disease
In July 1976, thousands of veterans gathered in Philadelphia for an American Legion jamboree. Hundreds stayed at the Bellevue-Stratford hotel. A week later, legionnaires throughout Pennsylvania fell ill. This drew the attention of the media, the public and the US Centers for Disease Control (CDC). Researchers mapped the legionnaires’ movements, studied the patients, and tested the hotel’s food, water and, eventually, air conditioning systems.
The CDC team suspected the hotel’s rooftop water coolers, which stood in proximity to the drinking water supply. The team saw rod-shaped bacteria in cell samples from infected people, but dismissed them as anomalies. They searched for a virus.
Faced with the publicity nightmare of a disease from the Dark Ages appearing in 20th-century Los Angeles, it is little wonder that the first instinct of the city’s civic leaders and their press allies was to obfuscate.Mark Honigsbaum
But it was bacteria – Legionella pneumophila – that linked the outbreaks. The hotel cooling towers were the breeding ground.
Legionnaire’s disease demonstrated that new epidemics can come practically out of nowhere. New environments – in this case, created by air conditioning and other technologies – produced a niche that an ancient, previously harmless disease could exploit.
AIDS
The second-deadliest pandemic of the 20th century – AIDS – began in the 1970s, but science did not identify it until 1980. Young, otherwise healthy men manifested a rare pneumonia, dying in droves. To date, the HIV retrovirus has killed more than 50 million people.
Honigsbaum expresses outrage that politicians ignored AIDS. The author believes that only stories about movie star Rock Hudson going to France for treatment spurred the government to release funds for AIDS research.
AIDS incubates, often without symptoms, for about 10 years while its carriers infect others. Advanced medical equipment and techniques allowed researchers to distinguish AIDS from an unknown pneumonia that had killed its victims for decades.
If Legionnaires’ disease had been a warning to an overly complacent public health profession, then AIDS was the epidemic that drove home the lesson. Mark Honigsbaum
Today people can live with AIDS, but uncomfortably, with the support of a daily drug cocktail.
Ebola
Experts erroneously regarded Ebola as insufficiently virulent to spread to African cities, let alone to the world. Poor communications spawned animosity between African villagers and visiting medical teams. A lack of medical infrastructure, the absence of infectious disease labs, a slow response by the World Health Organization (WHO) and local leaders’ denial of the facts escalated the contagion, as did West African burial rites calling for mourners to have close contact with the deceased. Fully 29,000 people suffered infection, and 11,000 died.
Not If – When
The past century brought frequent, unprecedented epidemics and pandemics that proved experts and conventional wisdom wrong each time.
Reviewing the last 100 years of epidemic outbreaks, the only thing that is certain is that there will be new plagues and new pandemics. It is not a question of if, we are told, but when.Mark Honigsbaum
New plagues, Honigsbaum makes clear, will continue to emerge.
Good Timing
Honigsbaum’s in-depth reportage arrived at exactly the moment when everyone wanted to know more about pandemics and how to cope with them. Wisely, the author doesn’t attempt to impress laypeople with medical arcana. He prioritizes the human element in every one of these tragedies, and he celebrates the heroes of this story – health care workers, medical researchers and scientists – who stand between humanity and pandemic catastrophe. Honigsbaum writes of how people make the same mistakes over and over, and how those mistakes foment terrible diseases. The foremost mistake, the author finds, is ignorance. Honigsbaum seeks to keep readers from succumbing to the errors of ignorance and succeeds in this gripping, fascinating and frightening read.
Mark Honigsbaum also wrote Valverde’s Gold; The Fever Trail; Living With Enza; and A History of the Great Influenza Pandemics.